Neurons in the brain coexist with and rely on many other cell types to function properly. Astrocytes, which take their name from their star shape, ensure the survival of neurons by feeding and detoxifying them with the help of a multifunctional protein, APOE. One of three forms of this protein, APOE4, significantly increases the risk of developing Alzheimer’s disease, but the mechanisms at play are unknown.
A collaboration between the University of Geneva (UNIGE), the European Molecular Biology Laboratory (EMBL), the University of Zurich and the pharmaceutical company AbbVie has discovered a potential mechanism: far from ceasing to function, APOE4 is on the contrary more efficient. By triggering astrocytic lipid secretion, it causes the accumulation of potentially toxic lipids that are harmful to neurons, and thus might contribute to the development of Alzheimer’s disease. These results published in the journal
Cell Reports, shed new light on the neurodegenerative mechanisms of a disease that affects nearly 50 million people worldwide.
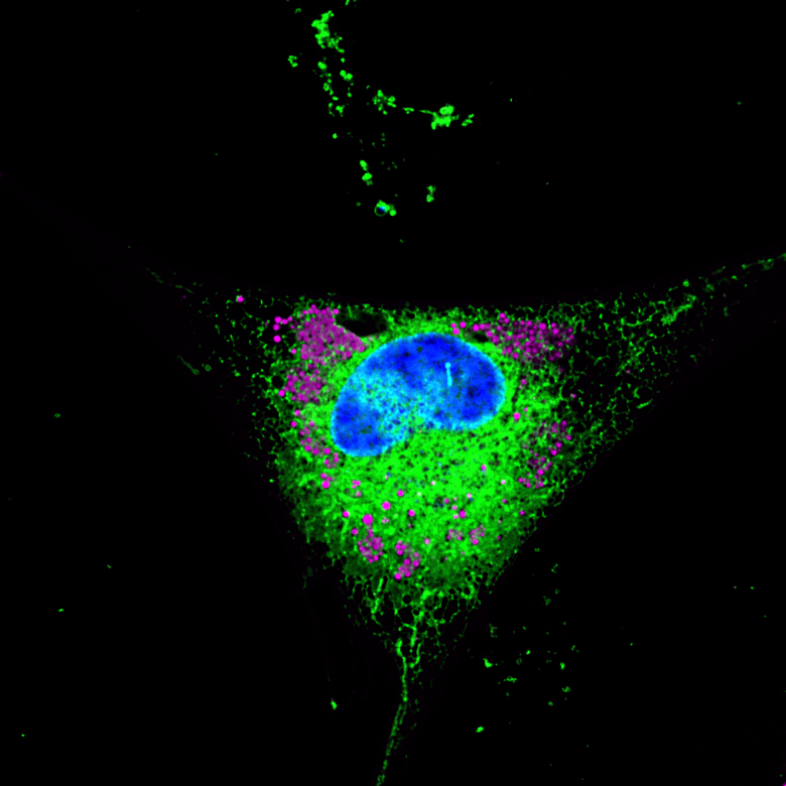
Astrocytes, present in very large numbers in the brain, have a major protective function. These cells secrete apolipoprotein E (or APOE), a small protein that forms particles containing lipids and vitamins to feed the neurons. It also detoxifies the neurons by getting them rid of “lipid waste” that could become harmful if not removed. As the neurons are unable to eliminate this waste on their own, APOE comes into play to collect it and bring it back to the astrocytes where it is destroyed.
The gene coding for APOE exists in three frequent variants in humans: APOE2, present in 8% of the population, APOE3, the most common, and APOE4, which is found in nearly 15% of people and increases the risk of developing Alzheimer’s disease by a factor of ten. “The reasons why APOE4 increases the risk of Alzheimer’s disease so significantly are not well understood,” explains Anne-Claude Gavin, a professor in the Department of Cell Physiology and Metabolism at the UNIGE Faculty of Medicine and holder of a Louis-Jeantet Foundation Chair, who directed this research together with Viktor Lakics, a Research fellow and Biology Area Leader in Neuroscience discovery at AbbVie. What are the mechanisms behind the dysfunction of APOE4? And above all, could they serve as a basis for prevention or therapy? To answer these questions, Anne-Claude Gavin and her team joined forces with scientists from the European Molecular Biology Laboratory (EMBL), the University of Zurich and AbbVie.
A protein that is too effective
Working on these questions, the research team identified novel molecular mechanisms that explain how APOE binds to astrocyte membranes to detect and extract the lipids it needs. Employing human cell lines with different APOE variants, in vitro experiments demonstrated that APOE is very efficient at transporting potentially harmful lipids produced in neurons. “And to our great surprise, the APOE4 variant proved to be even more efficient than the other forms”, reveals Katharina Beckenbauer, a former post-doc in Anne-Claude Gavin’s group, senior scientist at AbbVie, and one of the first authors of the work. “So, contrary to what we thought until now, the problem is not that APOE4 stops working, but, in fact, the opposite. And the mechanism goes haywire.”ici, le problème n’est pas qu’APOE4 cesse de fonctionner mais l’inverse: le mécanisme s’emballe.»
A hijacked function
As astrocytes age, they become less efficient and start to accumulate lipids rather than destroy them. “We modelled this process experimentally and observed the molecules secreted by the astrocytes,” explains Karina Lindner, a PhD student in Anne-Claude Gavin’s laboratory and one of the first authors of this work. “We observed that cellular ageing diverts APOE from its primary function — transporting lipids to neurons and also recovering lipid waste from them - towards the secretion of triglycerides, particular lipid species that could become harmful if not removed.” And this phenomenon is exacerbated with APOE4: it stimulates the secretion of triglycerides, leading to their uncontrolled accumulation. This deleterious accumulation of potentially harmful lipids could very well be an important contributor to the neuronal death, a hallmark of Alzheimer’s disease. “APOE4 would thus have the capacity to accelerate the pathological process in the disease through the mechanism we have discovered.”
In order to better understand the details of the action of APOE and especially of the E4 variant, the scientists at UNIGE want now to determine how secretion of these potentially harmful lipids is regulated and whether this secretion can be detected in people suffering from Alzheimer’s disease.

Faculty Diabetes Centre, Faculty of Medicine, UNIGE

Faculty of Medicine UNIGE


